Introduction to Skin Xenograft and HCMV
Skin xenografts have emerged as a fascinating area of study in modern medicine, particularly when it intersects with the complexities of human cytomegalovirus (HCMV). The combination of these two elements opens up new avenues for understanding transplant biology and immunology. Researcher Megan Loyd has been at the forefront, exploring how HCMV plays a pivotal role in skin xenograft outcomes.
As scientists delve deeper into this relationship, they uncover layers of complexity that challenge existing paradigms. What does HCMV mean for graft rejection? How can we leverage this knowledge to enhance patient care? Join us on this journey to unravel the intricate connections between skin xenografts and HCMV through cutting-edge research and innovative medical strategies.
The History of Skin Xenograft in Medical Research
Skin xenograft research dates back to the early 20th century. Scientists sought alternatives for human skin grafts, particularly in treating burns and wounds. Early attempts utilized animal skins, primarily from pigs and cows.
As techniques advanced, researchers began refining methods to enhance compatibility between donor tissues and recipients. The aim was always to reduce rejection rates while maximizing healing potential.
By the 1980s, skin xenografts gained traction in clinical settings. Surgeons used them during reconstructive surgeries with promising results. However, the challenge of immune rejection remained a significant hurdle.
In recent years, studies have shifted focus towards understanding how viral infections influence graft acceptance or rejection. This led researchers to explore various pathogens like Human Cytomegalovirus (HCMV) as possible factors impacting outcomes in skin xenograft procedures.
Through this historical lens, we can appreciate how far we’ve come—and where we’re headed in medical science’s quest for better solutions.
Understanding the Role of HCMV in Skin Xenograft Rejection
Human cytomegalovirus (HCMV) plays a significant role in the rejection of skin xenografts. This virus, prevalent in many individuals, can trigger immune responses that complicate transplant outcomes.
When foreign skin is introduced into a recipient’s body, HCMV may activate various immune pathways. These pathways lead to inflammation and tissue damage. Essentially, the body’s defenses perceive the graft as a threat.
Research indicates that patients with prior HCMV infection have varying responses post-transplant. Some exhibit heightened rejection rates compared to those without such infections. Understanding these dynamics is crucial for improving transplantation success.
Furthermore, HCMV interacts with other viruses and pathogens within the host. This interplay could influence how effectively the body accepts or rejects new skin grafts. Addressing this complexity may enhance patient care strategies moving forward.
Current Studies and Findings on the Connection between Skin Xenograft and HCMV
Recent research has delved into the intricate relationship between skin xenografts and human cytomegalovirus (HCMV). Studies reveal that HCMV may influence graft acceptance or rejection, highlighting its role in immunological responses.
Researchers have noted elevated levels of specific immune markers in patients with HCMV infections post-xenotransplantation. This suggests a direct correlation impacting graft longevity.
Innovative approaches are being explored to mitigate these effects. Some studies are testing antiviral therapies alongside transplantation procedures to improve outcomes for recipients.
Moreover, genetic profiling of both donor tissues and recipient immune systems is becoming a focal point. Understanding this interplay could lead to tailored treatments that enhance graft survival rates while minimizing complications associated with viral infections.
Insights gained from recent findings may pave new pathways for patient care in transplant medicine, emphasizing the significance of considering viral presence during such procedures.
Potential Applications of this Research in Modern Medicine
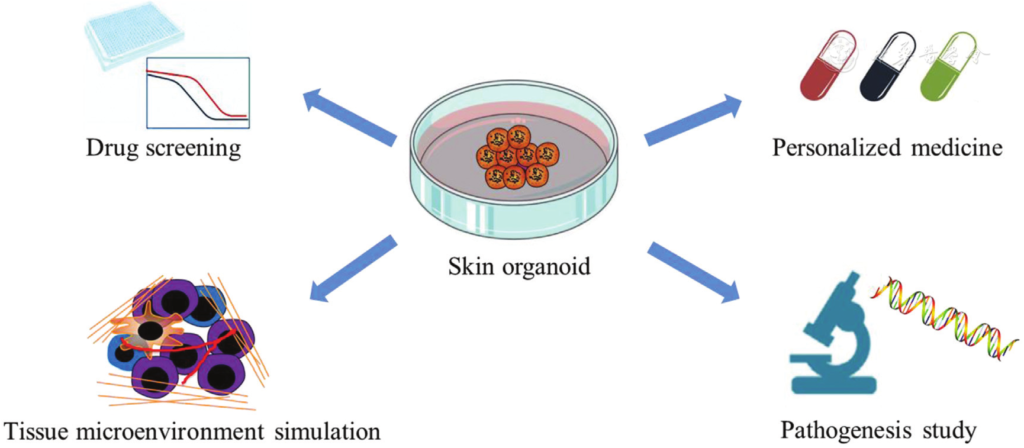
The insights gained from the study of Skin Xenograft HCMV Megan Loyd could lead to groundbreaking applications in modern medicine. Understanding how human cytomegalovirus (HCMV) affects skin xenografts offers potential strategies for improving transplant outcomes.
With enhanced knowledge, clinicians may develop targeted therapies to mitigate rejection rates. This could be particularly valuable for patients undergoing organ transplants or extensive skin grafts due to burns or injuries.
Additionally, exploring this connection might pave the way for novel approaches in immunotherapy and regenerative medicine. By harnessing the body’s immune responses more effectively, physicians can tailor treatments that promote acceptance of foreign tissues.
Furthermore, these advancements can extend beyond dermatology, influencing practices across various medical fields where tissue transplantation is critical. As research progresses, we may witness a significant shift in patient care standards and treatment methodologies.
Challenges and Limitations of Studying Skin Xenograft with HCMV
Researching the connection between skin xenografts and HCMV presents several challenges. One major issue is the variability in immune responses among individuals. Each patient’s body can react differently, complicating study outcomes.
Another hurdle is the ethical implications of using human tissues for research. Ensuring consent and maintaining a high ethical standard are crucial but also limit sample sizes.
Furthermore, HCMV’s latent nature makes it difficult to track its influence on xenograft rejection. Researchers often struggle with quantifying viral load and understanding its timing relative to graft acceptance or failure.
Environmental factors add another layer of complexity. External variables like infection rates or immunosuppressive therapies can skew results, making it hard to isolate specific influences of HCMV on skin xenograft success.
Funding constraints may restrict innovative approaches needed for deeper insights into this intricate relationship. These limitations highlight the need for more robust methodologies in future studies.
You Might Also Like:
- Discovering Yellow Roundhouse Katie: Insights and Fun Facts
- Unlocking the Secrets of Ancient Artz
- What Are the Benefits of Using Moszacos Lipstick Moisturizing?
Conclusion: Future Directions for Advancing our
The exploration of Skin Xenograft and HCMV opens new avenues for research in modern medicine. As studies continue to unfold, the implications for patient care become clearer. The relationship between HCMV and skin xenograft rejection holds potential not just for understanding transplant rejections but also for improving graft acceptance rates.
Future directions will likely focus on better understanding the mechanisms at play within this connection. Researchers may delve deeper into how HCMV influences immune responses during skin transplantation. This could lead to innovative strategies that enhance graft survival while minimizing complications related to viral infections.
Moreover, advancements in genetic engineering and immunotherapy may play a significant role in managing these challenges. Personalized approaches based on individual patient profiles might be developed, allowing tailored treatments that address both xenograft success and viral management.
As we move forward, collaboration among virologists, immunologists, and transplant surgeons will be crucial. By sharing insights across disciplines, the medical community can deepen its understanding of Skin Xenograft and HCMV interplay.
With continuous research efforts, it’s possible that future breakthroughs could significantly improve outcomes for patients requiring skin transplants—making strides toward more effective treatments rooted firmly in science-driven innovation.

